Note for Happy Hour on 7th April 2021
Thank you all who attended our last Happy Hour on the 7th April. And apologies for the lateness of this note on our meeting – it has been a busy time, but the content of our last meeting is, I believe very important, so better late than never, I hope – especially for those who did not attend the meeting.
Those of you who attended will know that we had our first specialist subject – Diverticulitis and were very fortunate to have Dr Christos Kontovounisios and Professor Gina Brown join us and present on this neglected, and very distressing, condition that can be a precursor to Colorectal Cancer. We don’t normally record our Happy Hour sessions as they are kept private to our RTD Community, with only my note on the RTD website with just the salient facts and news. However, this is such an important subject, that Christos has kindly agreed to re-present to video, so we will be posting that on the website in due course. In the meantime, I will try and capture key points on what we learned in this note.
Future presentations on specialist subjects may be recorded, with the permission of our presenters.
Now, a round up of our discussions last time.
Update from Professor Brown on PREVAIL and on Covid:
The PREVAIL project has succeeded well, with the FSSA – the Federation of Surgical Specialty Associations, comprising ten associations – approving the approach and looking at how to include the PREVAIL risk assessment method into the MDT (Multi-Disciplinary Team) processes and reporting.
Of course, acceptance by the FSSA is critical, but equally important is building awareness in the general public, and we heard from Professor Brown how the messaging on personal risk and timing – in getting seen and diagnosed, or happily reassured – is key to the success of the PREVAIL project. You will know that RTD is funding a PREVAIL video on the journey through diagnosis and treatment, aimed at the public, patients and clinicians.
Since our last meeting, work has progressed very well on producing the video, which has now been reviewed by a group of clinicians, GPs, NHS administrators and crucially by patients. More on this as it becomes reality, and we can use it to raise awareness. It will be on the RTD website in time, and we will ask you to share it widely as we see it as key to driving down deaths from Colorectal Cancer.
On Covid, Professor Brown told us that:
- Regular operating schedules were about to begin – from the 12th April,
- patients can now be scheduled in as normal, including day patients,
- elective surgical lists are also beginning,
- anaesthetic consultants are no longer needed in residence.
Of course, clinicians and patients are still being regularly tested and outpatients are continuing with virtual consultations unless it is necessary to be seen face to face. Professor Brown felt that PREVAIL being accepted will help those clinicians, dedicated to virtual telephone consultations, with the safe prioritisation of patients.
By the way, we also heard from Professor Brown a little known fact on the Covid vaccination front. Research into cancer vaccinations – yes, cancer vaccinations – contributed to the rapid development of the Covid vaccines! As if we needed another reason to continue supporting cancer research work by clinicians and scientists.
On Diverticulitis – what it is, its symptoms, diagnosis and treatment:
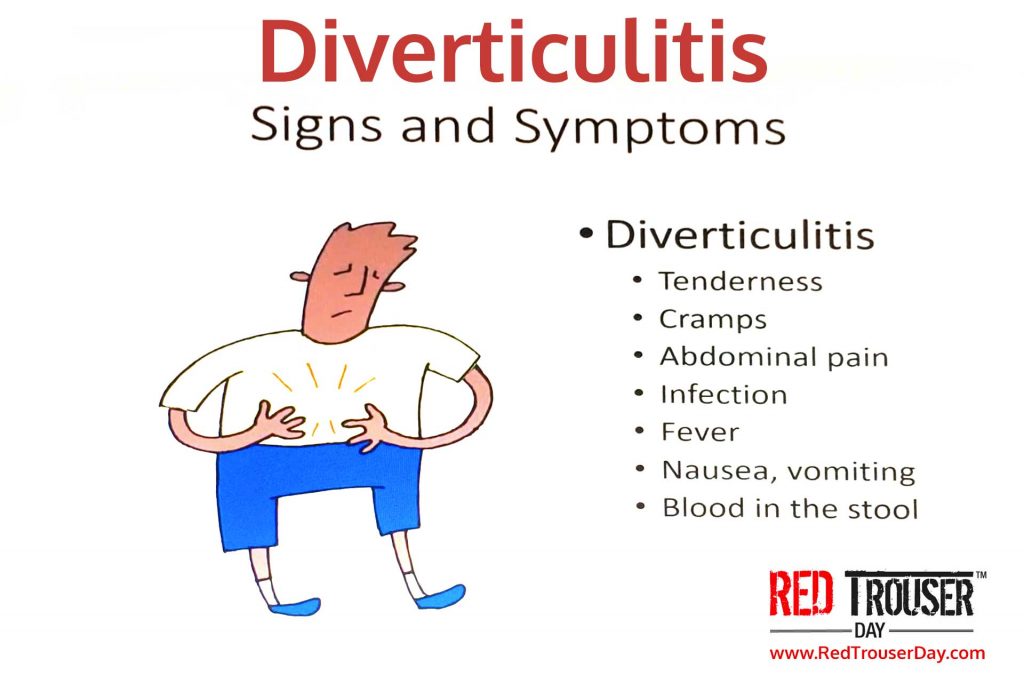 What it is and the symptoms
What it is and the symptoms
Dr Kontovounisios gave us a real tour around this condition – and what an education!
We learned that Diverticular Disease is caused by small sacs (diverticula) forming in the colon and bursting and sometimes bleeding – this is always on the left of the colon, where it is narrower, except in Africans, where it is often in the right colon.
Diverticula can be caused by constipation and their presence, known as Diverticulosis, is diet related and is silent with no pain – no symptoms at all. It is often picked up “by accident” when other investigations are being done, mainly through CT scans.
Treatment for Diverticulosis, or even mild benign Diverticulitis, is just an increase in fibre in the diet – we need to eat our greens! How many times did I hear that as a child?
The disease of Diverticulitis does cause abdominal pain (normally on the left), blood in stools, infection, fever and cramps. Even with these symptoms, the treatment can be fasting, to give the colon respite, followed by increasing fibre in the diet.
Diverticula can also occur in the duodenum (the first part of the small intestine, located between the stomach and the middle part of the small intestine). These are smaller sacs (bulges) in the duodenum and can also burst, beginning as small pinholes. This condition too can have no symptoms in the beginning, so early presentation is important. Treatment for duodenal diverticula is different from that for Diverticulitis, so what follows only applies only to Diverticulitis – found in the colon.
How it’s treated
So far, so good – being vigilant and aware can mean that we can manage Diverticulosis and even Diverticulitis fairly easily – with a healthy diet.
Dr Kontovounisios went on to tell us about Acute Diverticulitis – this is again picked up through CT scans showing inflammation and, in this case, bubbles of gas. Even at this stage, it is possible to settle it through a liquid diet accompanied by a course of antibiotics. Then, once settled, a patient would go on to have a colonoscopy – about 8 weeks from the original inflammation. About 25% of patients at this stage require more than just antibiotics.
So, if nothing changes after about 3 days, then a patient is straight into surgery, as Acute Diverticulitis can become an abscess and lead to massive bleeding, that is difficult to stop, and will need drainage. Also, while a scan can show a lot, it is not always possible to understand fully what is happening without an operation.
Just like the best horror movies, you didn’t think it could get worse – then it does!
Dr Kontovounisios described the complication of Fistulas forming, from the bowel, into other parts of the bowel or even other organs and areas of the body. The worst thing is that this can happen without manifesting many symptoms initially and the patient is only aware when they become very ill. If this happens, then the only treatment is complicated surgery, which may lead to an ileostomy – perhaps for life.
On the positive side, management of this condition has evolved and a combination of imaging, blood tests and genetic tests are used to individualise treatment – no one patient is the same, and Dr Kontovounisios told us how doctors are now trying much harder to tailor treatment. And, understanding of the microbiome, our “forgotten organ” is crucial. What is not recommended with Diverticulitis is taking laxatives!
The key message to us is to NEVER ignore symptoms as Diverticulitis can, if untreated, lead to death. Professor Brown advised us to go to our GPs, if we have symptoms, and ask for a colonoscopy. In fact, people with a genetic disposition to Diverticulitis or cancer, should be routinely checked through colonoscopy at an age of 10 years younger than an older relative who has had the disease, and Professor Brown advocates that everyone should routinely have a colonoscopy at the age of 50.
Why it occurs and how to avoid it
None of us are born with diverticula but diet, perhaps without enough fibre, can lead to pressure in the bowel and the formation of diverticula. It is more common in people over 40 years old, the obese and those not doing enough physical activity. So, just like eating all our greens, we need to walk more!
Of course, being constipated may have nothing directly to do with the bowel – it could be to do with pelvic floor weaknesses, e.g., resulting form the impact of pregnancy. This requires more than walking – it needs strengthening pelvic floor exercises.
Another key factor in keeping a healthy gut, and not developing diverticula, is hydration. Dr Kontovounisios urged us to drink plenty of water – apparently someone weighing 70kilos, needs between 2.5 and 3 litres of water a day!
Next Happy Hour:
Hope you enjoyed reading the summary of our last Happy Hour and that you will come to our next one, in less than one week’s time, on the 5th of May.
Our specialist subject in May will be, appropriately given what we learned in April, Nutrition.
Our guest will be Giovanni Ognio, licensed nutritionist from Perú specialized in High Performance Sports Nutrition & Plant – Based Nutrition, who is the head nutritionist and founder of LifeLifting, nutrition company from Lima, Perú working with patients from all around the world. He follows whole-food, plant-based diet patterns in his work.
He is proficient in Macro & Micronutrient interactions and biochemistry, being able to explain all this knowledge in a fun & easy way to understand. As a nutritionist, he loves being able to give expert advice to patients having an integral point of view, working to make them able to be the best version of themselves.
Giovanni has already worked with members of our family, including Paul, and transformed their gut health.