My name is Christos Kontovounisios, I’m a colorectal surgeon with an interest in cancer and complex pelvic examinations, and I’m an academic surgeon working at Imperial College and affiliated to the Chelsea Westminister, and the Royal Marsden hospital.
Today’s topic is about diverticular disease. I will give you an overview of the frequency, the prevalence of this problem, and how we can manage it – either with a conservative approach, or some surgical options that we have on everyday practice.

Mr Christos Kontovounisios
Clinical Senior Lecturer Consultant Colorectal and General Surgeon MD, PhD, FACS, FRCS
Terminology:
When we talk about diverticula it’s very important to understand a little bit on the definitions of these terms, these are medical terms, but they are quite common in everyday practice.
- Diverticulum is a sac-like protrusion of the colonic wall
- If you have many diverticula which don’t cause any problems, then this is what we call diverticulosis. you can live with diverticula without having any problems. We can see them either through images (X-rays) or through for example, a colonoscopy or an endoscopy. We know that they exist but they don’t cause problems.
- When there is an inflammation or another complication related to a diverticular, such as bleeding, then we use the term diverticulitis which means inflammation of the pockets.
Epidemiology
This condition or this disease it wasn’t common 100 years ago, and we know that with time the prevalence has increased.
Age:
It also has a different presence in different ages; it’s not so common in young age, but it’s quite common above the age of 60 or 85.
Gender:
There is a gender prevalence as well, depending on different age groups.
Diet:
but it is very much dependent on the diet, there is there is no strong evidence that there is a genetic predisposition, it’s very much dependent on diet. I’ll give you some examples later on differences between different continents and different countries.
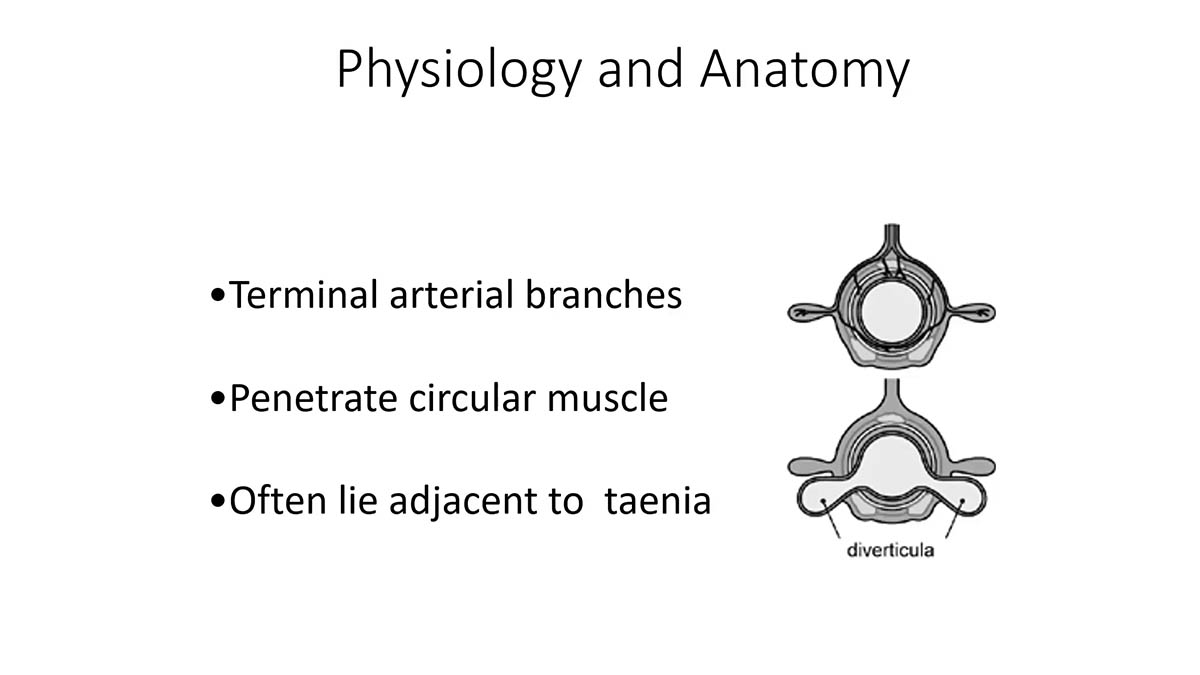
Physiology and Anatomy
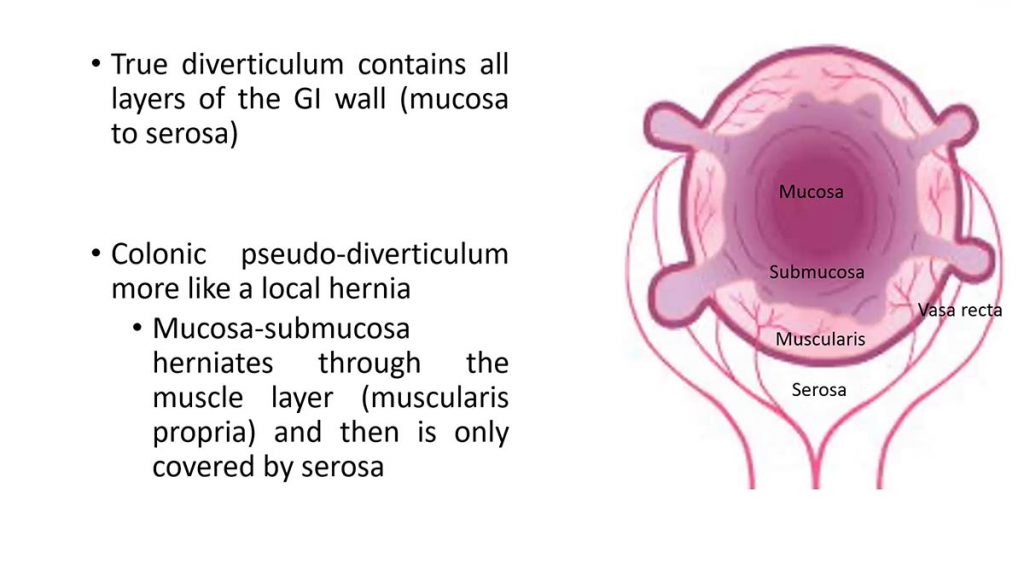
If you see on the picture is that there is a pocket on the outer layer of the bowel wall. We know that on the bowel wall there are some weak points, and weak points are where arteries can pierce through the bowel wall, and supply with blood the different layers of the bowel wall.
When the pressure inside the bowel either because of straining, or constipation, or slow transit – so it takes quite a long time for the faeces to travel from one side to the other side. The pressure builds up then through these weak points the inner lining of the bowel finds its way and creates an out pouch on the outer layer.
This is another picture of how the pockets may look like. The problem with these pockets is the wall is very thin. because it’s thin it can burst, and this is where the problems can start.
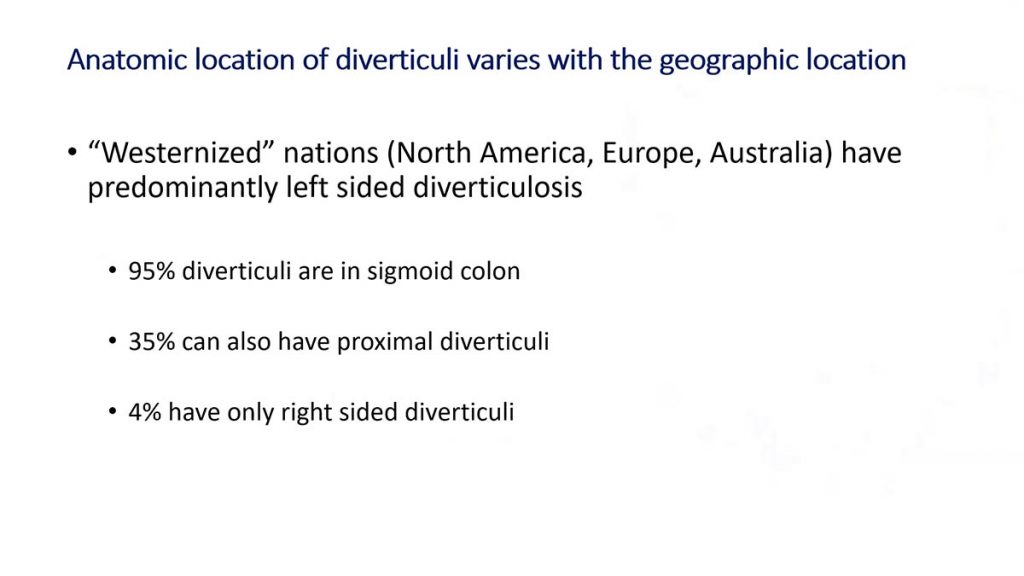
These problems are more common in Western nations, and that’s why the concept of lack of fibres, which is quite common a few decades ago in the western nations, is possibly the reason.
Lack of fibres means a greater chance of constipation which increases the pressure inside the colon, inside the bowel, and it can lead to the presence of diverticula.
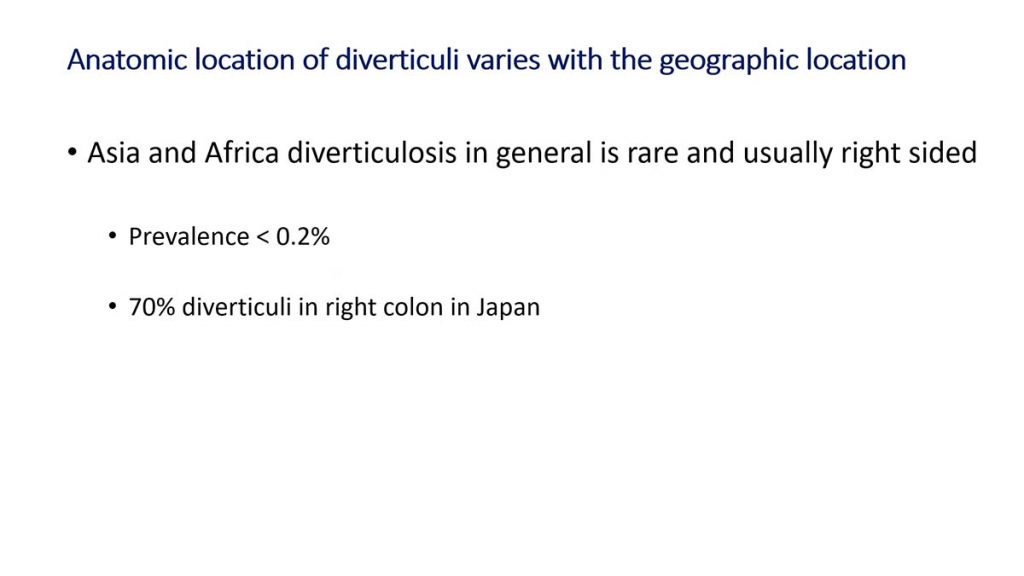
If you see other continents such as Asia and Africa the prevalence is very low which again fits with a theory of the lack of fibres in our diet. We know that low fibre can lead to diverticular disease, it’s not proven but it’s strongly suggested. The western diet is low in fibre and that leads to diverticulosis, while other countries don’t have this problem.
Obesity is associated with diverticulosis and especially men above the age of 40, and obviously lack of physical activity.
Signs and Symptoms of Diverticulosis
Most people have no pain or symptoms. The most common signs and symptoms of diverticulosis are:
· Diarrhea
· Constipation, so essentially you may have good and bad days, or changes on your bowel habits
· You may have heartburn
· Flatulence
· or sometimes you may have no symptoms at all.
Remember diverticulosis doesn’t necessarily mean there is a problem, but it does mean that there are diverticula in the bowel.
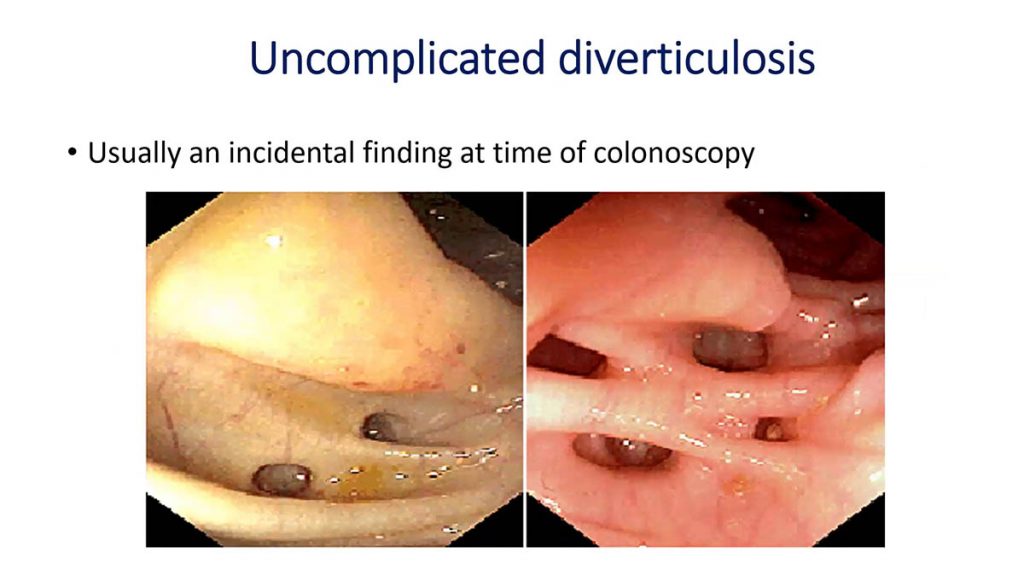
What do diverticuli look like?
This is from a colonoscopy where we see the bowel wall from inside, and you can see it’s like a small cave that protrudes outside and creates this out pouching.
On the right-hand side there is no redness around those pockets, so there is no associated inflammation this is what diverticulosis it’s called uncomplicated diverticulosis.
The second picture uses a contrast dye and an x-ray, and you can see where the arrows are these pouches again.
Uncomplicated Diverticulosis
We consider the diverticulosis as an ‘asymptomatic’ condition, but it can cause problems. To avoid those problems we if we know that the diverticula exists we have to be proactive by:
· changing lifestyle
· increasing fluid intake
· increase fibre intake
Making sure that we exercise on daily basis.
Common Signs & Symptoms of Diverticulitis
· pain in the left side of the abdomen where the majority of the diverticula are.
· Fever.
· On a blood test you will see raised inflammatory markers.
These are the three common signs and symptoms that can raise the suspicion of diverticulitis.
· we can also have cramps.
· blood in the stool – because as these pockets burst then the small blood vessels can cause bleeding.
If someone has lower abdominal pain, fever, shivering and on a blood test the raised inflammatory markers there is a strong suspicion of inflammation in the bowel from diverticulitis.
Diagnosis of Diverticulitis
This is the classic history that we teach our students how to diagnose someone with diverticulitis:
· The pain can vary depending on the presence of the diverticula and the inflammation.
· The pain ends up becoming constant it’s not colicky.
· The fever will become a problem in almost all the cases as the inflammation progresses.
Pain
It can be that there are previous episodes of pain without fever. So sometimes we do get early signs but we don’t really pay attention. But we should always think if we are constipated, there is a change in our bowel habits, and there are on and off pains in the lower abdomen, that should raise the suspicion that something is wrong with the with the colon in the bowel.
I would say that it’s the pain and the fever which are the two symptoms that should make a patient go and seek and advise, either with a general practitioner or to a colorectal surgeon.
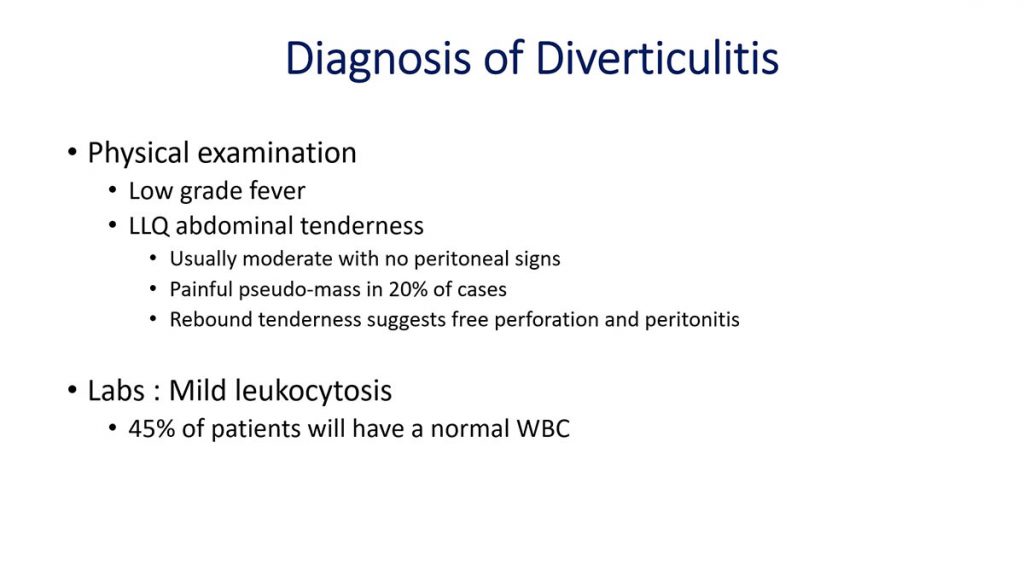
When we examine someone there will be sometimes a palpable mass in the lower abdomen. it might be very tender and painful, and sometimes you may have pain on the other side, on the right side of the upper abdomen if there is a lot of inflammation and fluid in in the tummy.
Sometimes patients can be in agony and cannot even breathe properly because of the pain, this is when we have generalised peritonitis. These are the extreme scenarios where patients need an immediate operation within a few hours.
On the blood test you will have increased inflammatory markers. but it could be that if it is a very early sign you don’t have massive changes.
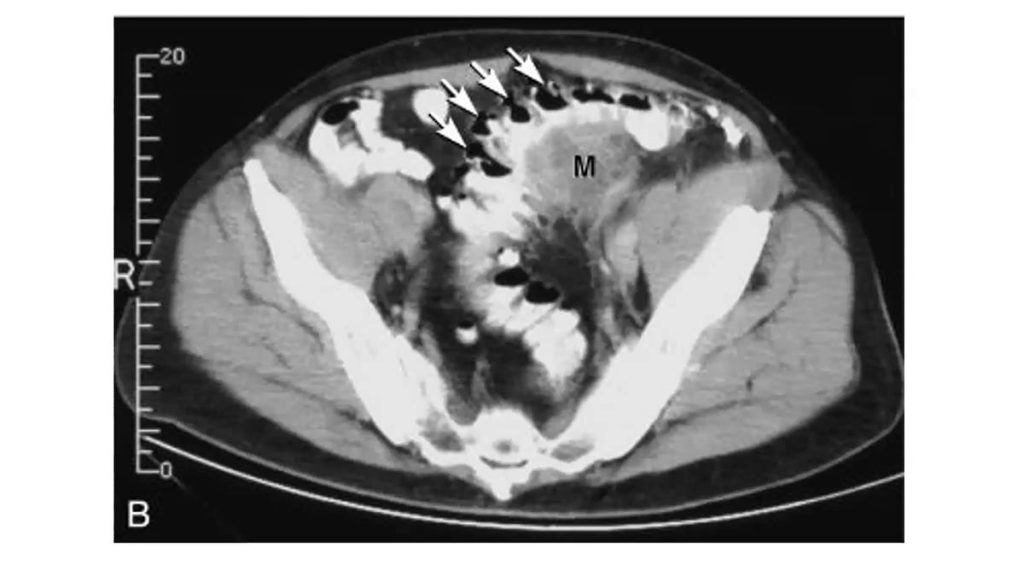
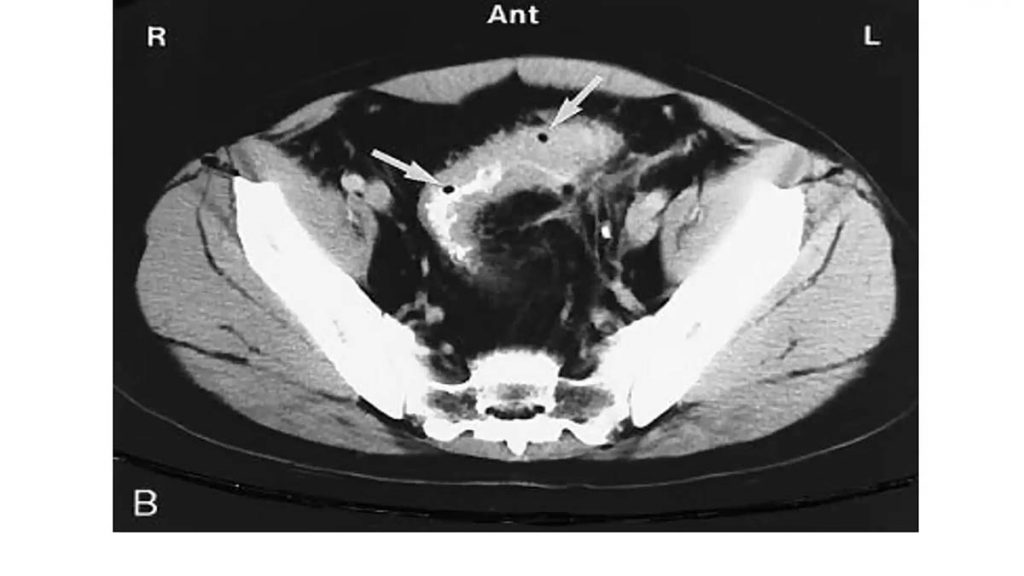
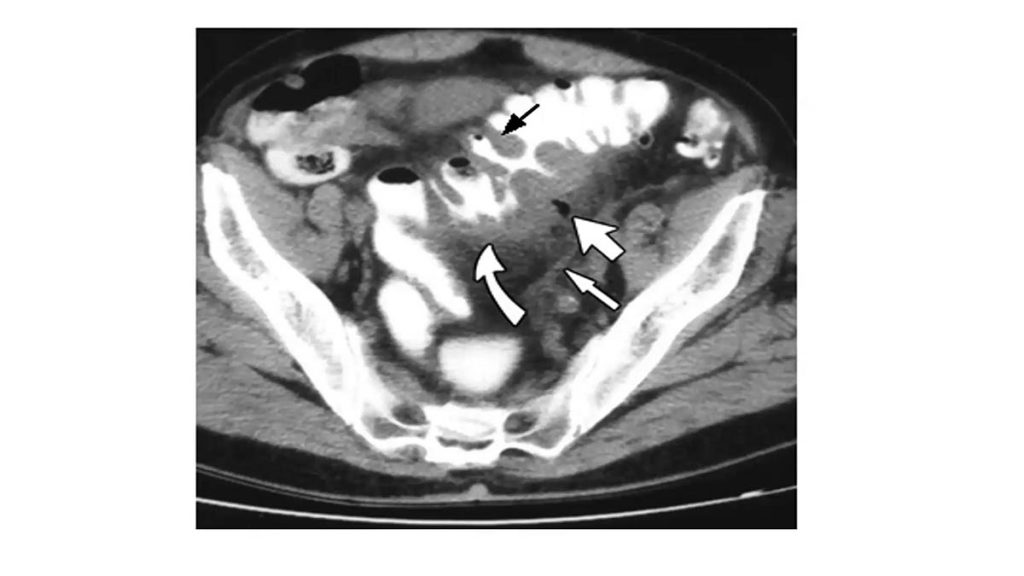
An example of Diverticulitis inflammation:
In the photo, where the arrows are, there is a lot of cloudiness around the white contrast inside the colon. This means inflammation around the bowel. This is how diverticulitis look.
This is another example where you can see locules of gas, these are what the two arrows demonstrate. So it means that the pocket has burst, and then gas from inside the bowel has escaped outside the bowl. This is a quite a serious problem because it means that there will be contamination outside the bowel, and the patient will be quite unwell.
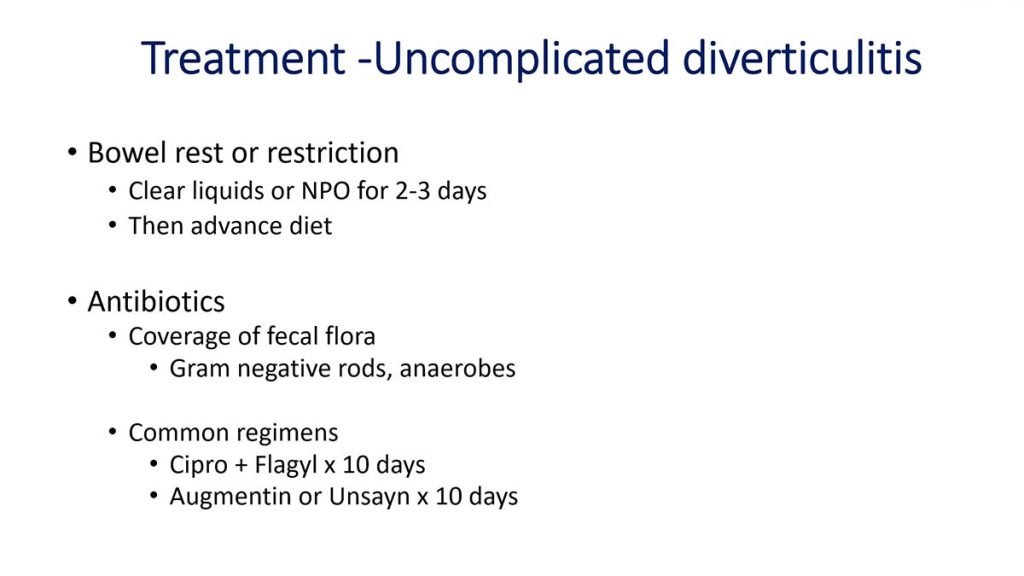
How do we treat diverticulitis?
How do we treat diverticulitis, the inflammation?
The first thing to do is we need to do is rest the bowel. We are not supposed to continue normal eating and drinking because the bowel then will keep moving and keep causing more problems.
So we need to completely rest the bowel, and that means fluids only. Sometimes even this is not the case and therefore patients have to have intravenous fluid to supplement their needs.
We have to start antibiotics, and what we commonly do (is use) broad-spectrum antibiotics that can cover most of the attacks of diverticulitis. The most common is a combination of antibiotics.
We need to monitor the patient very closely because things can change within 24 hours, or even 48 hours. If the symptoms fail to improve then a surgeon a colorectal surgeon has to be involved.
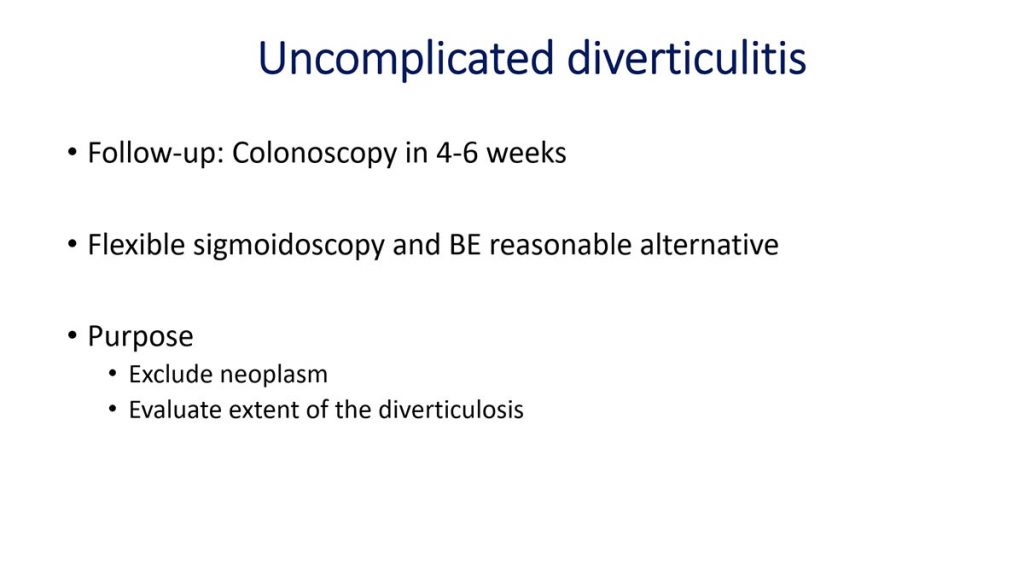
If everything settles down and there’s no need for an operation, what is very essential is to have a colonoscopy, to offer a colonoscopy to our patients, six weeks after the initial attack of the diverticulitis. The reason is there’s always a risk within that area of the inflammation to have another cause that has led to the picture that you see on a CT scan, such as cancer.
Colorectal Cancer
Cancer is not associated with diverticulitis, but you may have a polyp which may have cancer cells where the diverticula are. If you imagine that we make the diagnosis of diverticulitis with a CT scan and we see the bowel from outside it’s very important to estimate, and visualize the same problem whenever the inflammation settles down from inside the bowels, to inspect the inner lining of the bowel. That’s why we offer a colonoscopy at six weeks, because this is how much time the bowel needs to completely heal.
Sometimes if the problem is quite low, it’s close to the pelvis, a flexible sigmoidoscopy can be an option. This is to exclude the presence of cancer and also to have a baseline of the how extensive the diverticula are in the bowel.
Complicated Diverticulitis: Formation of an abscess
Another common complication of diverticulitis is the formation of an abscess. It’s a pocket of fluid, of puss that can develop next to where the pockets are. Imagine that there is an ongoing contamination through a small pinhole in the bowel and that can occur in about 15 to 16 percent of the patients with acute diverticulitis.
Complicated Diverticulitis: Formation of an abscess
Another common complication of diverticulitis is the formation of an abscess. It’s a pocket of fluid, of puss that can develop next to where the pockets are. Imagine that there is an ongoing contamination through a small pinhole in the bowel and that can occur in about 15 to 16 percent of the patients with acute diverticulitis.
There are different ways to treat this, sometimes antibiotics can be one. But sometimes you need to try to drain that abscess, to give an escape route for the fluid to come out and that’s why we use a CT guided drainage where we can insert small catheters where the abscess has formed, and allow the fluid to come out.
This is done by a specialised internal interventional radiologists. Sometimes we need to leave that drain for a long period of time but this way you avoid an operation which will mean removing part of the bowel.
Complicated Diverticulitis: Fistulas
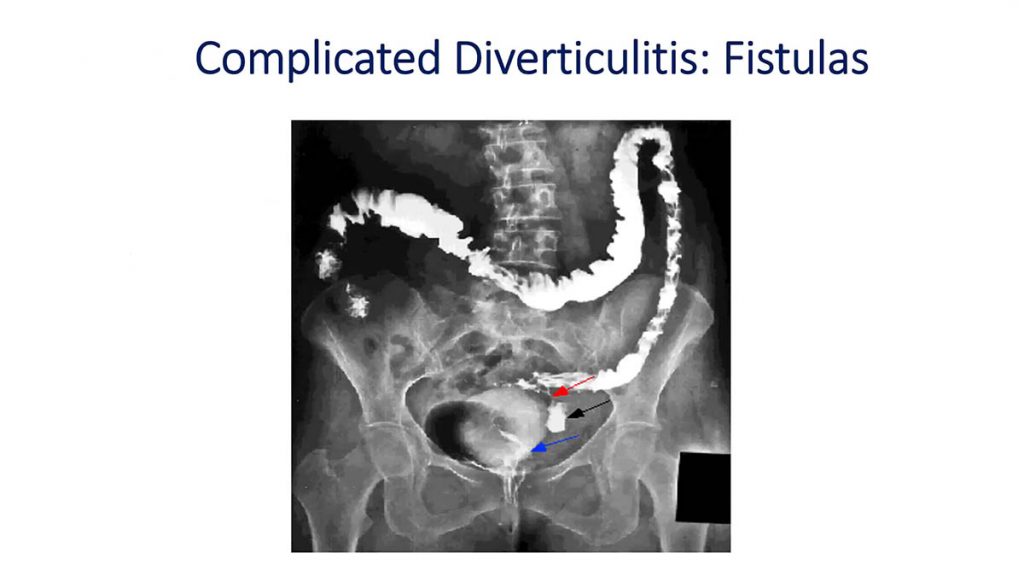
This is an example of how an abscess can become even bigger problem, which leads to what we call fistulas. Fistula is a communication between two organs.
In female patients you have next to the colon, next to the bowel you have the vagina, the uterus or the bladder. In a male patient you will have mainly the bladder, and the small bowel in both males and females. If there is an abscess which it happens to develop next between the bladder and the colon, then patients may have urinary symptoms more often. the reason is the contamination will go from the bowel to the abscess and will find its way to the bladder, and patients may have dysuria or pain or burning or what we call ‘new material’ where there is gas coming when we urinate.
The same can happen with the vagina or the uterus or other organs such as the small bowel. This is quite challenging when it comes to try to treat and monitor these patients, because it requires big operations which can lead to the need to have a diversion of how the feces come out with the formation of a stoma, which is not permanent but it is temporary.
This is the major types of different fistulas we can see in patients:
Treatment of Fistulas
Surgery is the option when we have such a complication which is the fistula, and that is to remove the part of the bowel which is affected, that has the inflammation and the abscess and the fistula.
Then we need to find the other end of that tunnel to the other organ and try to close that defect from the communication. If it’s the bladder, sometimes patients have to have a catheter that has to stay for a few days.
The surgical approach to diverticulitis is what we call the two-stage procedure, this is the most common practice which means removing the affected part of the bowel.
But you cannot join the bowel again together, if you try to make an anastomosis, a joint between the two ends of the bowel on the presence of inflammation that join will not be successful. There is a very high risk of the joint breaking down. That’s why we divert by creating a stoma where the bowel has to come to the skin, and the faeces enter into a stoma bag.
A minimum three months later, sometimes even longer, the patients will require another operation where you can join the two ends together.
Diverticular bleeding
The second most common cause of the presence of diverticula is bleeding. Many patients may present with bleeding, what we call hematochezia, which means presence of blood in the faeces.
It can be a really serious problem, and if you remember the diagram in the beginning, it’s those small blood vessels that burst and then they start bleeding. You also have usually elderly patients that they have medications with blood thinners for different reasons, and that can complicate the bleeding even more.
The majority of these bleeding points stop. It takes some time, the patients might need support either with blood products, or with fluids, or by resting the bowel but they stop.
There is sometimes a case where the bleeding doesn’t stop and we have to intervene. There is a risk of re-bleeding if we already have had bleeding, and this is up to 14 to 38 percent.
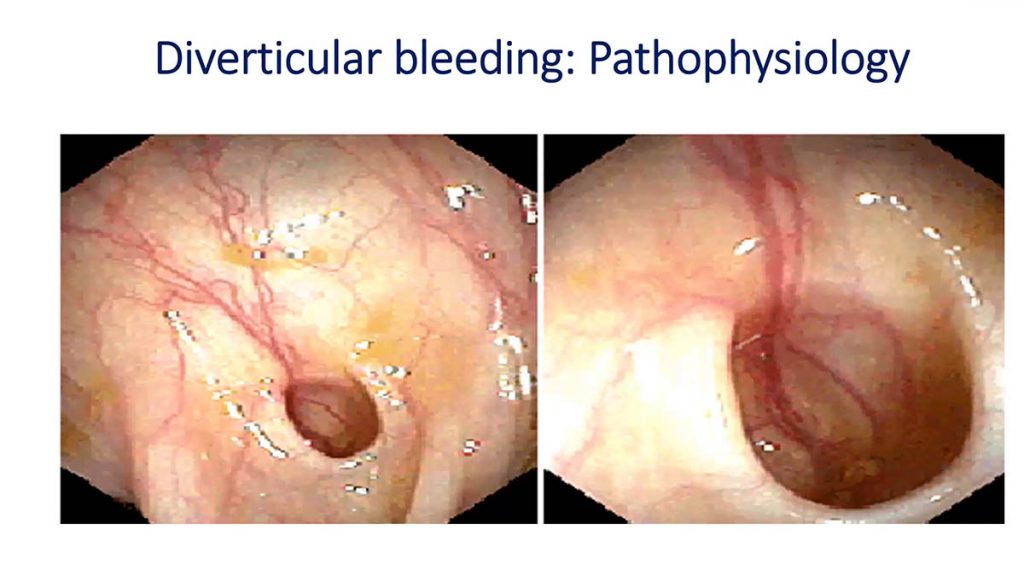
The photo shows a diverticulum, if you imagine these are the blood vessels that burst from the pressure, and then they start bleeding.
Diverticular bleeding: Symptoms
The main obvious sign is the presence of blood in the in the stool, and you don’t necessarily have pain and bloating and fever, it could be just bleeding.
There are also different sophisticated techniques if the CT scan fails to identify where the bleeding is. We have good sensitivities and specificities to localise if we have to operate, so we know which part of the bowel we have to remove.
Imagine if there is a true emergency where there is bleeding, but you don’t know, you can’t just remove all the bowel so it’s very important to localise where you have to operate.
Sometimes you can use endoscopic approach where you use you find that cave, you find that area, and then you can stop, you can cauterise, you use energy devices to stop a single bleeding point where the blood is coming from.
Diverticular bleeding: Management
The management is resuscitation, we perform images to localise where the problem is, we support the patients if needed with blood products.
If we have to we can with the CT (scanner) as a guidance, and with the expertise of interventional radiologists, we can embolise. We can find these bleeding points and stop them.
Diverticular bleeding: Surgery
If this becomes a surgical emergency you have different options. sometimes you remove part of the bowel, and again you cannot join, you have to do the two-stage approach where the patients have a stoma.
Sometimes you can’t join it depends on the patient’s background medical problems or other surgical problems, but the morbidity is high.
Conclusion
This is a summary of different signs symptoms and possible complications that someone might face with diverticula.
Thank you very much
Mr Christos Kontovounisios
Clinical Senior Lecturer Consultant Colorectal and General Surgeon MD, PhD, FACS, FRCS
Help us improve this page.
If you notice any errors or inaccuracies in this article please Contact us and let us know.
Copyright Notice.
- This article is distributed under the Creative Commons License Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0).
- You are Share — copy and redistribute the material in any medium or format for any purpose, even commercially.
- Attribution — You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
- NoDerivatives — If you remix, transform, or build upon the material, you may not distribute the modified material.
- No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.